20 year old male with massive spleenomegaly
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
roll no: 55
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case:
Chief complaints:
20 year male patient came to the casualty with the chief complaints of Neck pain since 2 days
Back pain since 2 days
Fever since 1 day
Blood in urine since 1 day(one episode)
HOPI:
Patient was apparently asymptomatic 2 days back then he developed neck pain which was of dragging type and insidious in onset and gradual in progression ,non radiating and relieved on medication( aceclofenac). It is not associated with vomitings, giddiness, rigidity and loss of consciousness. Back pain was in lower lumbar region and pricking type and was continuous. Fever was insidious in onset, low grade and relieved on medication.
Past history:
Patient had hypospadias and was corrected at 6 years of age.
Patient had facial puffiness and slight edema of lower and upper limbs at 12 years of age and was found to have anaemia and one unit of blood was transfused.
He had history of jaundice 10 days back
Not a known case of diabetes, hypertension, asthma, epilepsy, tb
Family history: no similar complaints in family
General examination
Patient is conscious ,coherent and cooperative .well oriented to time, place and person
Pallor present
Icterus present
No cyanosis
No clubbing
No lymphadenopathy
No oedema
Vitals:
Temperature:98.7 F
Pulse rate: 98bpm
Respiratory rate:19cpm
Bp: 120/80 mmhg
Spo2: 98% on RA
Grbs:152mg/dl
Systemic examination
Cvs:
S1 S2 present
No thrills
No murmurs
Respiratory system:
Vesicular breath sounds
Position of trachea is central
No dyspnoea
No wheeze
Abdomen:
Shape of abdomen: scaphoid
No tenderness
No palpable masses
No free fluids
Spleen: palpable below left coastal margin
Bowel sounds present
CNS:
Patient is conscious
Normal speech
No neck stiffness
Glasgow scale 15/15
Reflexes normal
Diagnosis:
Pancytopenia
Nutritional deficiency (vitaminB12 ? Iron deficiency )
With viral pyrexia
Investigations
20/12/22
Hemogram (19/12/22)
Hb: 6.0
Total count: 2,500
RBC:20.6
Platelets: 1.54
Reticulocyte count:0.6%
Serum iron:34ug/dl
Serum electrolytes:
Sodium:132
Potassium :42
Chloride :102
Calcium:0.93
Blood urea:30
Serum creatinine:0.7
Lft:
Total bilirubin:2.51
Direct bilirubin:0.40
Sgot:24
Sgpt:19
Alp:158
Total proteins:6.7
Albumin:4.1
A/g ratio:1.63
LDH:110
Dengue NS1 antigen: negative
Blood for dengue test: IgM : reactive on (18/12/22)
Peripheral smear:
Microcytic hyprochromic anemia with leukopenia
Direct and indirect coombs test: negative
Hemogram(20/12/22)
Hemogram (21/12/22)
Hemoglobin- 5.8gm/dl
Total count- 3,000cells/cmm
Neutrophils-40
Lymphocytes- 48
Eosinophils-02
Monocytes-10
Basophils-0
Rbc:3.63
Platelets-1.02
Smear:
Anisopoikilocytosis with microcytes macrocytes ,normocytes,with few target cells and pencil forms.
Hemogram (22/12/22)
Hb:5.8
TLC:2,400
RBC:3.64
Platelet count:1.52
Hemogram (23/12/22)
Hb:5.8
TLC:2,300
Rbc:3.55
Platelet count:1.36
LFT(23/12/22)
Total bilirubin:1.20
Direct bilirubin:0.31
SGOT:20
SGPT:29
ALP:165
Total proteins:5.6
Albumin:3.4
A/G ratio:1.65
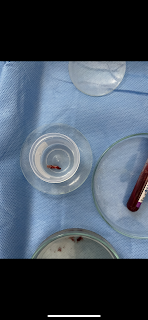
Bone marrow aspiration report
Hemoglobin electrophoresis:
Upper GI endoscopy:
Impression:
Atrophic fundal gastritis
Hemogram (24/12/22)
Hb:6.4
TLC: 3,000
Rbc:4.0
Platelet count:1.3
Bleeding time:2 mins 30 seconds
Clotting time:5 mins 00 seconds
APTT:40 seconds
PT:20 seconds
INR:1.4
LFT(24/12/22)
Total bilirubin:1.20
Direct bilirubin:0.31
Sgot:20
Sgpt:29
Alp:165
Total proteins: 5.6
Albumin:3.4
A/g ratio:1.65
Treatment:
19/12/22
Inj. Vitcofol 1500mcg IM/od
Tab hifenac p po bd
20/12/22
Inj. Vitcofol 1500 mcg im/od
Tab hifenac p po bd
Tab pan 40 mg po od
21/12/22
Inj. Vitcofol 1500mcg IM od
Tab hifenac p PO BD
Tab pan 40 mg po od
Inj FCM 500mg in 100ml ns /iv /stat
Tab pcm 1 gm po sos
22/12/22
Inj. Vitcofol 1500mcg IM OD
1 Ns @25ml/hr Iv
Inj iron sucrose 200 mg in 100 ml over 1 hr alternate days IV/OD
tab pcm 1gm po/bd
Tab. Pan 40mg po od
Tab. Buscopan po od
23/12/22
Inj. Vitcofol 1500mcg IM OD
1 Ns @25ml/hr Iv
Inj iron sucrose 200 mg in 100 ml over 2 hrs alternate days IV/OD
tab pcm 1gm po/bd
Tab. Pan 40mg po od
Tab. Buscopan po bd
24/12/22
Inj. Vitcofol 1500mcg IM OD
1 Ns @25ml/hr Iv
Inj iron sucrose 200 mg in 100 ml over 2 hrs alternate days IV/OD
tab pcm 1gm po/bd
Tab. Pan 40mg po od















Comments
Post a Comment