General medicine final practical short case
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
roll no: 45
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
This is a case of 50 years old patient, who is a farmer by occupation, resident of pochampally has presented to the casualty 7 days back with the chief complaints of
- Abdominal distension since 8 days
- Pain in the abdomen since 8 days
- Pedal edema since 6 days
5Am-Wake up
Till 8AM- Field work
8AM- Breakfast (Rice)
1PM - lunch
6PM- reaches home
8PM - dinner
9PM - sleep
The Patient was apparently asymptomatic 6 months ago when he developed jaundice and was treated in a private hospital
His last consumption of alcohol was on 29th May 2022 which was when he drank more than usual
Then he developed abdominal distension which was insidious in onset and gradually progressive to the present size
There were no aggravating and relieving factors
It was associated with
1)pain abdomen in the epigastric and right hypochondriac region which is insidious in onset and diffuse to whole of the abdomen and gradually increased in intensity and is of colicky type
Pain is persistent throughout the day. No history of radiation to the back.
2) bilateral pedal edema below knees and is of pitting type, which was insidious in onset and gradually progressive throughout the day and is maximum in the evening and is not relieved by rest
No local rise of temperature and tenderness
Associated symptoms- shortness of breath since 4 days
There is no history of orthopnoea, palpitations.
No history of facial puffiness and haematuria.
No history of evening rise of temperature, cough, night sweats.
No history suggestive of hemetemesis, melena, bleeding per rectum .
No raised JVP, basal lung crepitations.
No palpable mass per abdomen.
Past history
No history of of similar complaints in the past
Not a known case of Hypertension, Diabetes, asthma, epilepsy, TBNo previous surgical history
Personal historyDiet- MixedAppetite- Decreased since 10 daysBowel and bladder movements- RegularSleep- AdequateAddictions-Patient is a chronic smoker since 30 years- 4to5 beedis/dayAlcohol - Consuming whisky since 20 years- 3 to 4 times per week (90 ml each time)No history of drug or food allergies
Family historyNo similar complaints in the family
General examination:
Done after obtaining consent, in the presence of attendant with adequate exposure
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Patient is well nourished and moderately built
Pallor - absent
Icterus- present
Cyanosis- absent
Clubbing- absent
Pedal edema- present- bilateral pitting type.
Lymphadenopathy- absent .
General examination:
Done after obtaining consent, in the presence of attendant with adequate exposure
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Patient is well nourished and moderately built
Pallor - absent
Icterus- present
Cyanosis- absent
Clubbing- absent
Pedal edema- present- bilateral pitting type.
Lymphadenopathy- absent .
VitalsTemperature- AfebrileBlood pressure- 120/80 mm of HgPulse rate- 78 bpmRespiratory rate- 16 cpm
Local examinationAbdominal examination:
InspectionShape of the abdomen- DistendedUmbilicus- evertedMovements of abdominal wall- moves with respirationSkin is smooth, shinyNo visible peristalsis, pulsations, sinuses, engorged veins, hernial sites Palpation
Inspectory findings are confirmedTenderness is present in whole of the abdomenGuarding and rigidity presentFluid thrill positiveNo hepatosplenomegaly
PercussionFluid thrill- felt Liver span- Not detectable
AuscultationBowel sounds are heard
Cardiovascular system examination:S1 and S2 sounds are heardNo murmurs
Respiratory system examination:Bilateral air entry presentNormal vesicular breath sounds are heard
Central nervous system examination:No focal neurological deficits
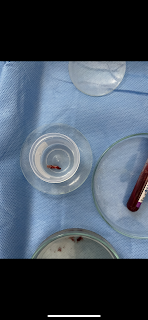
Investigations