General medicine final practical long case
roll no: 45
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case:
A 26 year old female from nalgonda who is a homemaker came to the hospital with the chief complaints of :
• Lower back pain since 15 days
• Fever since 10 days
History of presenting illness:
• The patient was apparently asymptomatic 15 days back, then she developed lower back pain which was insidious in onset and gradually progressive, and continuous dragging type which finally became severe pain. Pain is more during night time. The severity of pain is decreased after medication. The pain is not radiating .
• Then she developed fever 10 days back which was insidious in onset gradually progressive which was high grade and associated with chills and rigors.
• She also had history of vomitings. On day 1 of admission - 1 episode and on day 2 of admission - 6 episodes. They are yellow in colour, food as contents, not projectile. Relieved on medication.
• The patient had noticed red coloured urine before the day of admission and on the day of admission, which is not associated with pain or burning or difficulty in passing urine, no oliguria or increased frequency of micurition .
•She had facial puffiness and abdominal distension on day 5 of admission which later subsided.
• There is no history of chest pain, breathlessness, cough, indigestion and heart burn.
Past history:
At the age of 10years she was diagnosed with Rheumatic heart disease and she underwent a surgery (CABG and mitral valve replacement)following which she took medication for 2 years and she stopped using them thereafter ,and again she’s using the medication from past 7months.
No DM,TB,HTN,Epilepsy
Personal history :
Diet:mixed
Appetite:normal
Bowel and bladder movements:regular
Sleep disturbed due to pain
No addictions
No allergies
Family history :not significant
Menstrual history :
Age of menarche:13 years
5/28 cycle ,regular,moderate flow , with clots ,no dysmenorrhea
Marital history : married for 7 years 7months back gave birth to a girl baby.
General examination:
Patient is conscious,coherent and cooperative
Well oriented to time place and person
Moderately built and nourished
Pallor -present
No icterus ,cyanosis,clubbing ,generalised lymphadenopathy,edema
Vitals:
Pulse rate:70/min
RR:20/min
BP:120/70 mmHg
Temp:afebrile.

Fluid intake and output chart:

Systemic examination:
Per-abdomen examination
Inspection:
Shape of abdomen:normal
Movements:all quadrants are moving equally with respiration
C-section scar is present
No engorged veins ,sinuses,swellings
Striae gravidarum present
No visible gastric peristalsis
Palpation :
No local rise of temperature ,no tenderness
No palpable mass
No hepatomegaly ,spleenomegaly
Kidney not ballotable.
Percussion :resonant note heard
Auscultation : bowel sounds heard.
RESPIRATORY SYSTEM :
bilateral air entry - positive
Normal vesicular breath sounds heard
CENTRAL NERVOUS SYSTEM :
Higher mental functions are normal
Sensory and motor examinations are normal
No signs of meningeal irritation
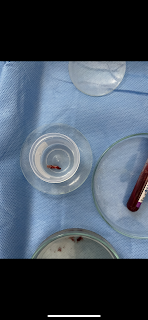
Clinical images:
CVS :
Inspection:
Midline scar is present
Shape of chest normal
No precordial bulge
JVP not raised
No visible pulsations
Palpation: Apex beat felt at 5th ICS 2.5 cm medial to mid clavicular line
Auscultation :
S1S2 heard no murmurs
Click sound is heard without stethoscope (replaced mitral valve ).
Investigations:
On Day1:
Hb:9.8 %
TLC:21,900
N:83,L:7,B:2,M:8
Platelet:2.1 lakh
Normocytic normochromic anemia
LFT:
APTT :51seconds
PT:25 sec
INR:1.8
RBS:101 mg/dL
Urea:26
Sr.creatinine :1.4
Na+:141 mEq
K+:3.4
Cl_:106
On day 4
Hb:10.1
Urea :18
USG :
(Done On the day of admission)
Impression:altered echo texture and increased size of right kidney
 2decho:
2decho:ECG:
X-ray:
Diagnosis:
Acute pyelonephritis
Treatment:
IV fluid -NS,RL :75mL/hr
Inj.piptaz 2.25 gm IV TID
Inj.pan 4mg IV OD
Inj. Zofer 4mg IV SOS
Inj.neomol 1gm IV SOS (if temp >101F)
Tab.PCM 500mg /PO/QID
Tab .niftaz 100mg /PO / BD (stopped)















Comments
Post a Comment